More than three in five UK adults are overweight or obese, increasing their risk of diseases such as type 2 diabetes and cancer.
In the UK, adults eat as many as a third of their meals out of home, including in workplace cafeterias, and these meals are often much higher in calories than meals eaten at home. Since April 2022, calorie labelling is now required on food and drink served out of the home in businesses employing 250 or more people. While many people welcome this information, evidence for its effectiveness in reducing calories purchased or consumed is limited in quantity and quality. For example, two previous studies conducted by the authors in nine worksite cafeterias found no evidence for an effect of simple calorie labelling (kcal) on calories purchased.
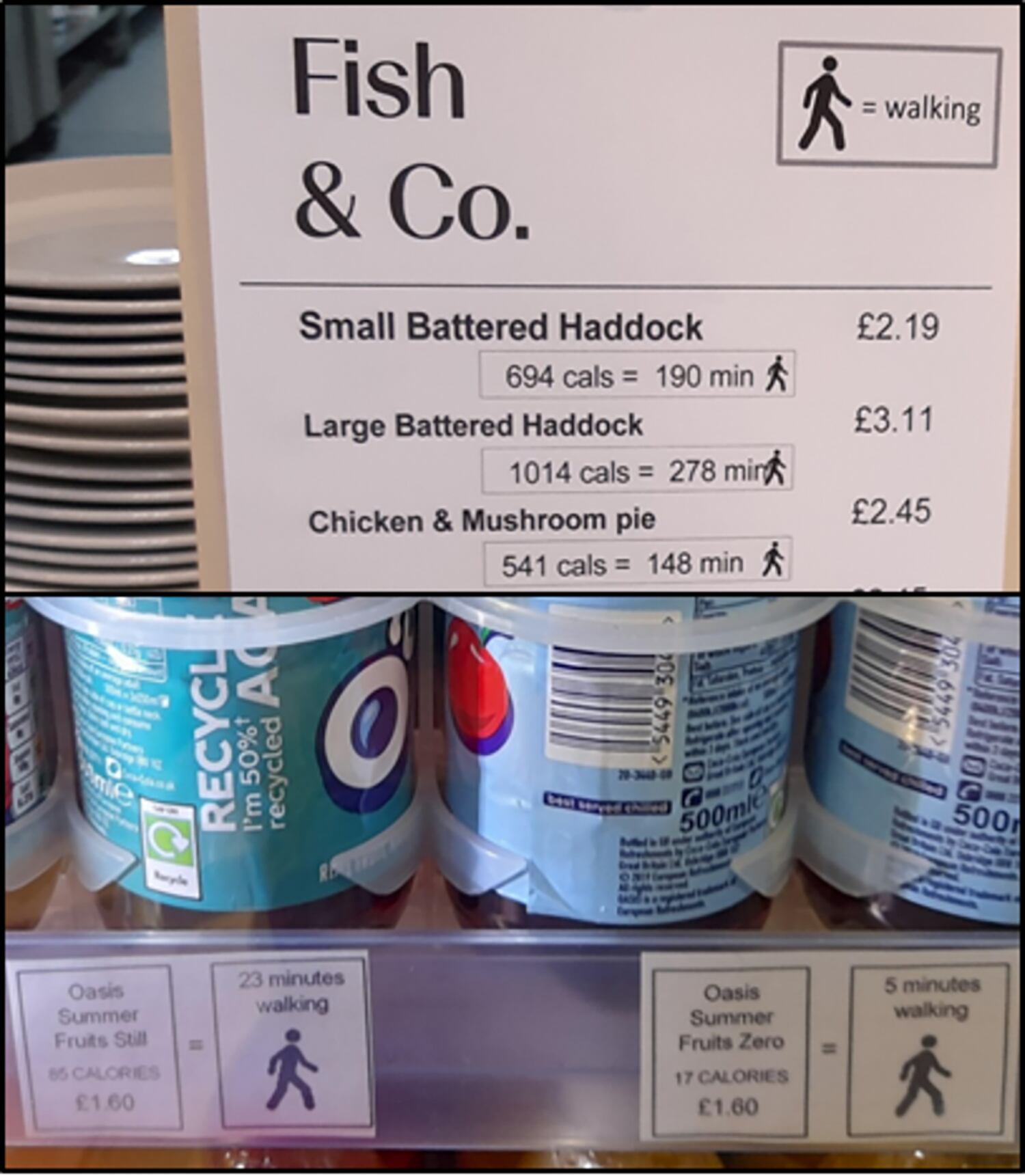
Some experts have called for the use of so-called PACE (physical activity calorie-equivalent) labels on food and drink products. These show the amount of exercise required to burn off calories.
A recent systematic review of the existing evidence concluded that PACE labels may reduce energy selected from menus and decrease the energy consumed when compared with simple calorie labels or no labels, but only one of the 15 studies reviewed was in a ‘real world’ setting.
To explore whether PACE labels can make a difference in real world settings, researchers from the University of Cambridge’s Behaviour and Health Research Unit placed PACE labels alongside food and drinks items in 10 workplace cafeterias in England over a 12-week period in 2021.
Items used in the experiment included hot meals, sandwiches, cold drinks and desserts. For example, customers were told a 1014kcal ‘large battered haddock’ portion would take over five hours walking (278 minutes) to burn off. Those who bought a chicken and mushroom containing 541 calories were told it would take 148 minutes of walking to burn off the meal.
The results, published in PLOS Medicine, revealed no evidence that including PACE labels resulted in an overall change in energy purchased from labelled items. However, there was a great deal of variability, with one cafeteria reporting a fall per transaction of 161kcal and another an increase of 69kcal, while five of the cafeterias reported no significant change.
First author Dr James Reynolds from the School of Psychology, Aston University, who carried out the research while at Cambridge, said: “Although we found that showing the amount of exercise required to burn off calories made little difference to the number of calories purchased – and, we can assume, eaten and drunk – there was considerable variability between cafeterias. This suggests that other factors may have influenced the effectiveness of these labels, such as the type of food sold in the cafeteria or the characteristics of those using them.”
The number of calories purchased from items that did not feature the PACE labels did not change and the labels made little difference to the revenue for the cafeterias – just a small increase of 3p per transaction.
Senior author Professor Dame Theresa Marteau, Director of the Behaviour and Health Research Unit at the University of Cambridge, said: “This is the largest study in a real world setting to look at the impact of PACE labels on food and drink purchases, examining 250,000 transactions across 10 worksite cafeterias. The findings suggest that PACE labels, contrary to expectations, may have little or no impact on the food people buy in worksite cafeterias.”
Reference
Evaluation of physical activity calorie equivalent (PACE) labels’ impact on energy purchased in cafeterias: a stepped-wedge randomised controlled trial
PLoS Medicine
DOI: 10.1371/journal.pmed.1004116


